Introduction: The challenge of diagnosing and definitively classifying myeloproliferative neoplasms (MPNs) and myelodysplastic/myeloproliferative neoplasms (MDS/MPNs) remains a conundrum in the field of hematology. While the World Health Organization has outlined diagnostic criteria for various categories, there remain cases that elude specific classification, falling under the umbrella of MPN, unclassifiable (MPN-U) and MDS/MPN, unclassifiable (MDS/MPN-U). In this study, we aimed to compare the morphological and genetic profiles of cases classified as MPN-U or MDS/MPN-U against more definitively classified cases (including chronic myelomonocytic leukemia (CMML), essential thrombocythemia (ET), MDS/MPN with ring sideroblasts and thrombocytosis (MDS/MPN-RS-T), and primary myelofibrosis (PMF), including prefibrotic PMF (pre-PMF)).
Methods: Morphologically unclassifiable myeloid neoplasm cases referred for pathologist review to our laboratory in the largest tertiary care center in British Columbia, Canada were identified through pathology database query over a five-year period. Bone marrow materials were reviewed and reanalyzed with standardized collection of qualitative and semiquantitative data by two hematopathologists. Morphological parameters studied included the myeloid to erythroid ratio, bone marrow cellularity, lineage dysplasia, megakaryocyte histotopography, bone marrow blast frequency, fibrotic changes, and bone marrow vascularity, among others. Clinical data, cytogenetic findings, and results of a targeted sequencing panel assessing a set of approximately 50 genes recurrently mutated in myeloid malignancies were collected by electronic medical record review. A cohort of contemporarily collected myeloid neoplasms with definitive pathologic diagnoses was reviewed for comparison. Statistical analyses were performed using python3.
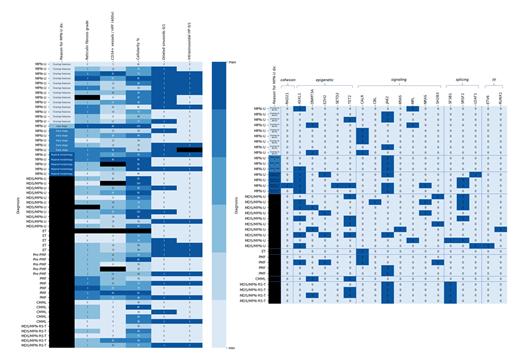
Results: The cohort comprised 29 cases classified as MPN-U, 12 cases of MDS/MPN-U, and 5 cases each of ET, PMF, pre-PMF, CMML, and MDS/MPN-RS-T. MPN-U cases were further subcategorized based on the apparent reason for difficulty in classification, including: overlapping features with another MPN; late stage/overt fibrosis; early stage without fully-developed morphologic features; and coexisting atypical morphologic findings. MPN-U with overlapping features had highly variable reticulin fibrosis, while, as expected, late stage entities had a high degree of reticulin fibrosis and early stage entities showed less overt fibrosis (Figure, Left, demonstrating select morphologic features of evaluated chronic myeloid neoplasms). MPN-U as a whole appeared to show less prominent fibrosis-associated findings than MDS/MPN-U and to, in general, show a greater degree of neovascularization, similar to changes observed in cases with PMF. Splicing factor and epigenetic modifier mutations appeared to be overrepresented in MDS/MPN-U relative to MPN-U, notably excluding MPN-U with atypical morphologic features (Figure, Right, demonstrating the distribution of pathogenic variants identified in evaluated myeloid neoplasms; results are indicated as presence (1) or absence (0) of a variant for each gene). Notably, no CALR mutations were identified in the MDS/MPN-U category or early stage / atypical morphology MPN-U, though they were enriched in overtly fibrotic MPN-U entities.
Discussion/Conclusion: In this cohort we observed, as expected, significant overlap in cases classified as MPN-U and MDS/MPN-U with better delineated entities, though patterns of morphologic change and mutational spectra suggest potential directions for further investigation of additional criteria that may guide accurate classification of these neoplasms. These findings reflect the heterogeneity of MPNs described in the literature and the complexity of their genetic underpinnings, particularly in the context of concurrent dyshematopoiesis; suggest enhanced bone marrow vascularization may be an informative differential diagnostic criterion in evaluation of these neoplasms, though further study is required; and emphasize the need for broader genetic testing and perhaps further subtyping of MPN-U cases for a more nuanced analytical approaches for these disorders.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal